If the phased and fluid approach of returning to worksites seems at times frustrating, it’s because the typical process is dependent on many factors. These include the number of local COVID-19 infections, employers’ tolerance for risk, readiness of policies and protocols, and employees’ willingness to walk back in the workplace doors. Additionally, there’s the recent surge in cases in many states and localities, along with varying conditions for resources such as personal protective equipment (PPE) and testing capabilities.
As a result, for some organizations it has been ready, set, false start. Or sometimes, “Let’s just wait.”
While uncertainties abound, employers can follow a playbook to have greater confidence in their game plan for getting workers back on site appropriately. A well-planned approach includes key elements such as:
- Preparation
- Testing and tracing
- Providing care and support
Preparation
Being prepared includes several considerations as shown below and informed by guidance from the Centers for Disease Control (CDC).
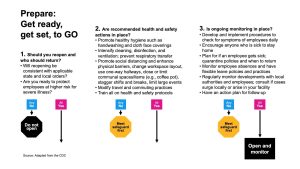
Step 1: Define who will return and when.
Some decisions depend on the ability to provide adequate protections. Clearly, office workers in close cubicles cannot maintain safe social distancing and, in turn, cannot return to side-by-side seats. If it’s impossible to reconstruct the physical space to separate desks or devise physical screens or barriers, employers may need to limit occupancy, consider staggered shifts and work weeks, and/or work with employees as to who returns and when.
Employers also need to be cautious in setting policy to not run afoul of federal, state, or local legislation, even if acting under the belief that workers are being protected. For example, it’s known that older workers and those with underlying health conditions who contract COVID-19 are at risk of more severe outcomes. However, an employer can’t simply tell older workers not to return, as that would be prohibited under the Age Discrimination Employment Act (ADEA).
Still, an employer can educate workers on risks and allow them to choose to return vs. continuing to work at home (if that option works within the parameters of the employee’s job duties). If self-selection is not possible, employers should carefully review work needs, accommodations, absence or leave policies, resources and support (physical, as well as mental and emotional), and consult with counsel to be sure there is no bias.
Step 2: Develop policies and protocols.
As highlighted in the above visual, health and safety steps range from setting behavioral expectations, reducing unnecessary proximity, and enabling touchless interactions. Indeed, facilities managers have been busy posting educational and warning signage (“be cool, follow the six-foot rule”), applying stepped-up cleaning and sanitation, using Plexiglas or other barriers to promote social distancing, changing office workflow, restricting some communal areas, and more.
Some buildings are adapting elevators to have antibacterial covers on buttons or use of touchless card keys to access one’s office floor. Some elevators even sense the number of people who have entered and automatically close the doors after two or four.
Other examples of plan elements include:
- Triage processes and referral channels for care if an employee has symptoms or a positive test result
- Decisions on requiring and supplying personal protective equipment (PPE)
- Decisions on testing vendor credentials and protocols
- How education and training will be presented and updated
- Policies for various what-if situations, including exposure, isolation, treatment, and subsequent return to work
Step 3: Monitor at individual and organizational levels.
Many companies are requiring employees to conduct a self-assessment of symptoms, with varying levels of formality and technology. For instance, certain apps involve checking symptoms, whereby employees cannot enter the building without a pass on their device. Additionally, some employers include temperature checks upon entry. Still others are using aggressive, ongoing testing. A comprehensive plan acknowledges that managing the virus requires never vacillating on vigilance.
At the organizational level, plans must address employee illness or reports of employees whose family members may be infected. Employers also must stay abreast of local conditions and surges..
At the same time, companies must educate employees to be attentive and know what to do if they or a household member has been exposed or if they believe they are infected. This leads to the next key step in well-defined policies, including testing, but it also incorporates guidance for self-quarantining and requirements for safely returning to work (typically at least 14 days ,but preferably with medical guidance, especially if the infected person demonstrates any symptoms).
Testing and Tracing
Employers have implemented a variety of action plans to support testing. Under the CARES Act, all health plans must cover the costs of testing and treatment. Some employers are fortunate to have onsite or nearby testing sites. Others need to make it easy for employees to know where to go if they suspect exposure and a COVID-positive result. Challenges also remain in finding labs to turn around testing results in a timely manner.
It’s also worth mentioning that the ability to screen for antibodies has driven considerable conversation, expert guidance now suggests that antibody tests should not be used to determine an individual’s immunity, or readiness to return to work.
Meanwhile, tracing is highly sensitive from a HIPAA protection standpoint; dialogue with legal counsel is advisable to proceed with caution. Nonetheless, you may consider hiring contact tracers, as well as technology tools with GPS capabilities to help with social distancing and understand exposures.
Providing Care and Support
Employers can make a difference in the health of workers and families with training on new protocols and evolving insights. Ongoing messaging can raise awareness and prompt taking responsibility for informed action.
Employees also may not realize that the care they take on the job is only helpful to the extent they take the same care off the job to protect themselves and their families. In turn, your education ideally will extend to sharing knowledge with the home. Communication channels such as mobile-friendly microsites and pop-up sites, ideally with no required password to enable family access, can help educate and provide rapid updates, especially if outbreaks occur. You should update content frequently as the situation and protocols evolve.
Care and support also must recognize that employees have extenuating circumstances in their lives, like caregiving for children or elderly relatives. Likewise, some employees may have family members who have lost jobs or wages. Employee assistance plans, wellbeing resources, and supportive managers can help.
Additionally, some people may fear for their own jobs, leading them to take risks by coming to work while possibly infected. Emphasize that their priority must be their own and others’ health and safety. If they have been exposed to the virus, they need to know there will not be adverse consequences if they come forth and get guidance on quarantining for a time.
Ultimately, COVID-19 playbooks continue to evolve in responding to the pandemic and returning employees in good and sustainable good health to the worksite. Each employer’s situation is unique, but informed and flexible checklists, documentation, and education plans can help achieve the thumbs-up needed for (and from) employees to return to the workplace with greater confidence.
